Main focus
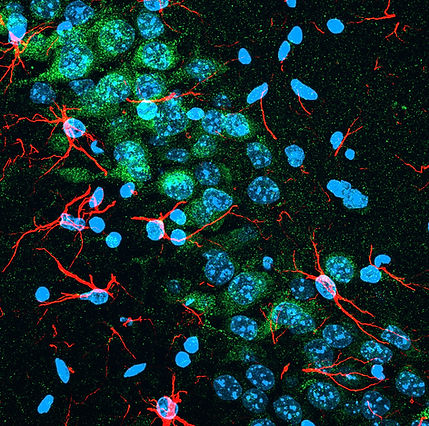
The group’s PI Anna Malik has extensive experience in studying various aspects of cell biology, in particular signaling pathways and intracellular signaling. In the past, she worked on the mechanisms important for the pathogenesis of brain disorders including epilepsy, Alzheimer’s disease, and ischemic stroke. She has been working of the activities of different cells of the brain (neurons, astrocytes, microglia) and how they contribute to shaping the properties of brain microenvironment.
Now, we take advantage of this background to investigate the mechanisms controlling the activities of the cells present in the brain and their impact on the microenvironment and the pathogenesis of brain diseases. We focus mostly on the astrocytes, microglia, and macrophages infiltrating the brain in pathological states.



VPS10P receptors in glia
Glial cells, in particular astrocytes and microglia, play a key role in reacting to any brain disease or damage. In response to pathological changes in the brain, glial cells undergo activation leading to the secretion of biologically active proteins that may control the immune response, stimulate production of new blood vessels or rebuild the extracellular matrix, i.e. the substance surrounding the cells. Intriguingly, glial cells may behave differently in the course of distinct diseases, which is associated with the secretion of various proteins, and in consequence leads to a variety of effects, promoting recovery or, on the contrary, stimulating inflammation and destruction of nerve cells. Acquisition of these distinct properties by glial cells depending on the type of stimulus is called phenotypic polarization. This process, which triggers various states of microglia and astrocyte activation, is extremely important for the course of brain diseases, but the mechanisms controlling it are still not fully understood.
We propose that the activity of so-called VPS10P domain receptors may contribute to different glial cell functions associated with phenotype polarization. VPS10P receptors, which include SorLA, sortilin, SorCS1, SorCS2 and SorCS3, are present in the brain and are known primarily for their function in neuronal cells. They contribute to the proper sorting of proteins inside neurons, i.e. they direct their protein ligands to the appropriate cellular compartments. As a result, the target proteins reach the appropriate location within the cell or are secreted to the extracellular space. We expect that VPS10P receptors may also perform similar functions in astrocytes and microglia, thereby contributing to the secretion of proteins crucial for the disease progression.
Our aim is therefore to determine the importance of VPS10P receptors for glia function in various activation states and, in consequence, for the course of brain diseases. We plan to explore mechanisms controlling the level of VPS10P receptors in astrocytes and microglia and to uncover new proteins sorted by these receptors and secreted by activated glial cells. Finally, we will examine the importance of these processes for the pathogenesis of brain diseases such as gliomas, Alzheimer's disease or ischemic stroke.
This project is financed by the National Science Centre (OPUS program, 2020/37/B/NZ3/00761; Preludium program, 2023/49/N/NZ4/01690, and by the I.3.4 Action of the Excellence Initiative—Research University Programme at the University of Warsaw.


TET2 in stroke
Stroke is one of the leading causes of death worldwide and often leads to lifelong disability. In this project, carried out by an international consortium, we investigate the role of so-called clonal hematopoiesis in ischemic stroke (i.e. stroke caused by occlusion of a cerebral vessel with subsequent blockade in blood flow). Clonal hematopoiesis, in turn, is an imbalance of circulating blood cells that occurs more frequently with age and is a risk for both tumor development and vascular events such as stroke. If hematopoietic stem cells mutate, this might lead to overgrowth of certain cells that is called clonal expansion. Of note, patients who have clonal hematopoiesis caused by acquired mutations in the gene TET2 are at higher risk for a second vascular event or death in the future. What is completely unknown, however, is whether such clonally expanded blood cells, as they occur in clonal hematopoiesis, can enter the brain after a stroke and cause additional brain damage.
We now want to investigate the impact of TET2-related clonal hematopoiesis on post-stroke events. Mice with different levels of clonally expanded Tet2-mutated blood cells will be exposed to an experimental stroke. Subsequently, we will investigate the migration of the mutant cells into the brain, the resulting tissue damage in the brain as well as the functional recovery of the animals. In a second step, we will then specifically treat these animals with clonal hematopoiesis with drugs that block inflammation. Our group will characterize the functional consequences of Tet2 loss in the context of the secretory activities of macrophages. Finally, we will elucidate molecular mechanisms behind the regulatory roles of TET2 in macrophages.
This project is financed by the Eranet Neuron / The National Centre for Research and Development (NeuronC2/II/34/CH-Stroke/2023.



CHI3L1 in post-stroke regeneration
Stroke is a serious health issue and one of the top causes of death and long-term disability in adults. The most common type is called ischemic stroke, which happens when blood flow to a part of the brain gets blocked. This blockage reduces oxygen and glucose supply, leading to death of neurons and activation of other cells of the brain, including astrocytes. Currently, treatment options for stroke mainly focus on restoring blood flow, but they often fail to prevent lasting brain damage. This damage can lead to a range of disabilities, affecting movement, vision, speech, and swallowing. After a stroke, the brain undergoes inflammation and tissue remodeling that have great impact on regeneration and rehabilitation.
Astrocytes, a type of brain cells, play a key role in responses to brain pathologies, including stroke. After an ischemic stroke, astrocytes become active and gather around the damaged area. They release important substances that can influence how other cells in the brain respond to injury, which has important consequences for the regeneration after stroke. One of the substances released by astrocytes is called chitinase-3-like protein 1 (CHI3L1), also known as YKL40. For a long time, CHI3L1 was only seen as a sign of inflammation, but recent research shows it may play a much larger role in brain health. It appears to affect various processes, including inflammation and the growth of new blood vessels, which are important for recovery after a stroke.
While higher levels of CHI3L1 in the blood seem to be associated with worse outcomes after a stroke, it is still debated whether blocking CHI3L1 could help improve recovery. Thus, in the research project, we aim to explore whether blocking CHI3L1 can aid recovery after stroke. We will investigate how CHI3L1 influences cells in the brain after ischemic injury and how astrocytes release this protein. We hypothesize that CHI3L1 released by astrocytes affects the healing processes after stroke. We propose that blocking CHI3L1 might help avoid excessive inflammation and support better healing. To test these ideas, we will use both animal model of stroke and cell culture models. We will investigate the impact of a CHI3L1 blocker on various levels, including recovery of motor skills after stroke. We will employ various techniques, like observing improvement of motor skills in animals after a stroke and analyzing the properties of the cells in the brain.
In summary, by combining advanced research techniques and experimental models, we hope to uncover how CHI3L1 influences the brain’s response to stroke and the recovery. This knowledge could be crucial for finding new treatment options for stroke patients in the future.
This project is financed by the the National Science Centre (SONATA Bis program, 2024/54/E/NZ4/00134).



Disrupted SorCS2-dependent neuronal protein sorting in epileptic encephalopathy
Epileptic neonatal encephalopathy is a severe neurological disorder characterized by epileptic activity and progressive cognitive, behavioral, and sensory impairments in full-term infants. Recent advancements in genetic research have led to the identification of variants of genes associated with epilepsy, sparking interest in understanding the underlying mechanisms. Our collaborative study with researchers from the University of Alberta, Canada, led to the identification of a novel mutation, c.2614C>T (p.Pro872Ser), in the SORCS2 gene in full-term newborns with epileptic neonatal encephalopathy (Ambrose et al., 2025).
SorCS2 is a neuronal receptor that regulates intracellular trafficking, membrane protein recycling, and synaptic plasticity. It interacts with key targets like BDNF, TrkB, and p75NTR, influencing neurotrophic signaling, axon growth, and neuronal survival. SorCS2 modulates glutamatergic signaling by regulating the surface expression and recycling of NMDA receptors, which are essential for excitatory neurotransmission. In glutamatergic neurons, SorCS2 regulates the cell surface levels of the excitatory amino acid transporter EAAT3, whose dysregulation is associated with epilepsy.
Our functional studies in Hek293 cells revealed that the new identified mutation affects SorCS2’s dimer formation, a key process for its proper function, and impedes SorCS2 typical localization in Rab11-positive recycling endosomes. We hypothesize that the altered SorCS2 function and its impact on receptors and transporters recycling contributes to epilepsy by disrupting glutamatergic and/or neurotrophin signaling, which can lead to disrupted neuronal development and abnormal neuronal activity. To test this hypothesis, we plan to use human neurons derived from induced pluripotent stem cells, to examine the functional consequences of the c.2614C>T mutation and SorCS2 knockout. The project will utilize organoid models as well, which will provide a complex and physiologically relevant context by allowing the study of the phenomenon from the cellular to the tissue level.
Our project aims to investigate how SORCS2 mutation and knockout affect human neuronal development, activity, and protein recycling, and to assess the response of these cells to standard anti-seizure drugs as potential therapeutic strategies. Using a broad spectrum of experimental approaches such as live neuron imaging, RNA sequencing, quantitative mass spectrometry, and microelectrode arrays to monitor neuronal activity, we will determine whether SorCS2-dependent disrupted protein sorting, altered surface protein levels, or abnormal interactions between mutated SorCS2 and its targets contribute to epilepsy phenotype.
This project is financed by the National Science Centre (SONATINA program 2025/56/C/NZ5/00217).




